Before antibiotics, millions died each year of diseases we can easily treat today. If we’re not careful, we may be headed back to those deadly days.
In 1928, Alexander Fleming discovered that a fungus, Penicillin rubrum, could kill bacteria. But his fellow doctors wouldn’t listen.
It wasn’t until 1943, when he cured a patient dying of meningitis in just one week, that they finally paid attention.
Fleming won the Nobel Prize but cautioned that bacteria could grow resistant to penicillin—if the patient took too little or for too short a time.
Again, people didn’t listen. And did what he warned against.
Just 20 years later, some bacteria had evolved to resist penicillin, including strains of pneumonia and Staphylococcus—the staph infection that plagues hospitals today.
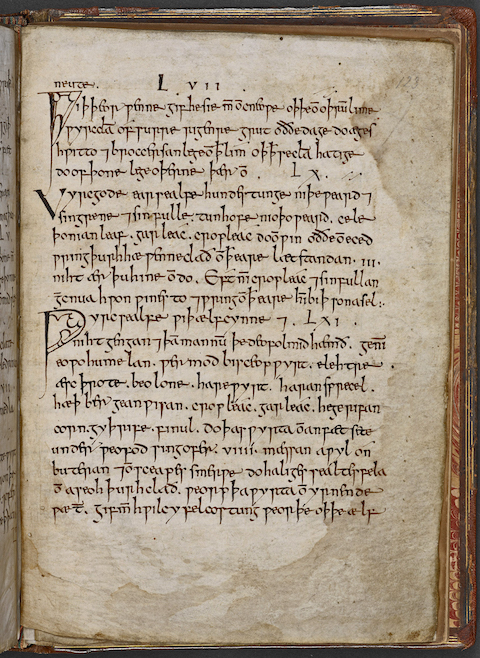
Desperate scientists have searched everywhere for something to help, including thousand-year-old medical texts. Among potions to ward off elves and night goblins, they found a salve made of cow bile, wine and herbs that actually fights the deadly staph. Today a commercial version is available.
Meanwhile, improper antibiotic use continues to breed superbugs. But, you can help. If you’re prescribed antibiotics, finish the entire dose.
If not, you could be training new strains of bacteria—that won’t respond to medieval folk cures.
Background
Synopsis: One of the world’s most urgent healthcare issues is the emergence of pathogens that have evolved to defeat antimicrobial treatments. In 1928, Alexander Fleming discovered penicillin, and by the end of World War II the drug had revolutionized medicine, making former deadly diseases treatable. However, insufficient doses administered over decades have enabled bacteria to evolve resistance to the drug, creating supergerms that leave humans defenseless. Amazing recent studies of medieval potions demonstrate that a 1,000-year-old salve may come to the rescue. If concocted exactly per the recipe, it conquers the superbugs.
- Before the advent of antibiotics, millions succumbed to bacterial infections like bacterial endocarditis, meningitis, pneumococcal pneumonia, gonorrhea, and syphilis. In the late twentieth century, these infections were treatable with penicillin and other antibiotics.
- In September 1928, Scottish doctor and microbiologist Alexander Fleming noticed a culture plate with an open lid in one of his lab experiments. It had been contaminated by a fungus that had destroyed the Staphylococcus aureus colonies he was studying. The fungus was Penicillium rubrum.
- It took him about 15 years to convince other scientists of its efficacy against bacterial infections, which killed millions each year.
- In 1942, he used penicillin to cure a friend of life-threatening streptococcal meningitis in just a week and published the results in The Lancet in 1943.
- With World War II underway, the British Ministry of Health and the War Cabinet authorized urgent mass production of the drug for use by Allied troops before D-Day (6 June, 1944).
- In 1945, Fleming shared the Nobel Prize in Physiology or Medicine with two colleagues for the discovery and development of penicillin, ushering in the age of modern medicine.
- Even as he accepted the Nobel Prize on 26 June, 1945, Fleming warned that “the microbes are educated to resist penicillin...In such cases the thoughtless person playing with penicillin is morally responsible for the death of the man who finally succumbs to infection with the penicillin-resistant organism. I hope this evil can be averted.”
- Early experiments had shown Fleming that certain species of bacteria would develop immunity to penicillin if too little was used or if it was used for too short a time (that is why your doctor asks you to complete the full course of antibiotics).
- By 1942, strains of Staphylococcus aureus had evolved to survive exposure to penicillin, and by the 1960s, most strains of this virulent species were resistant.
- In 1967, Streptococcus pneumoniae had developed resistance to penicillin.
- Since then, additional germs have developed antibiotic resistance, assaulting every organ and increasing the dangers of surgery and implants.
- Every year more than 2.8 million Americans are infected, and more than 35,000 of these patients die of their antibiotic-resistant infections.
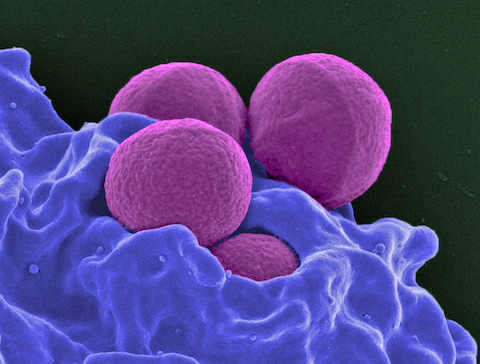
Scanning electron micrograph of a human neutrophil ingesting MRSA (Methicillin-resistant Staphylococcus aureus) Credit: National Institute of Allergy and Infectious Diseases (NIAID) - These types of infections impact people of all ages, animals and even plants and are one of the world’s most urgent health care concerns.
- In the search for novel alternative remedies for deadly infections, researchers have delved into ancient medical manuscripts like the Old English Bald’s Leechbook.
- In addition to potions and salves for injuries and infections, some of the Leechbook’s remedies address supernatural concerns: one salve is said to protect the user from elves (ælfcynne), night goblin visitors (nihtgehgan) and devils (deofol).
- Other mixtures were more practical, especially Bald’s eyesalve. Scientists brewed up 75 batches from garlic, onion, leek, cow bile and wine, varying the varieties of garlic, onion and leek.
- The resulting mixtures are antiseptic and some formulations are highly effective at killing antibiotic resistant Staphylococcus aureus (MRSA), even when the supergerm forms sturdy clusters called biofilms.
- Breaking up biofilms to get at individual bacteria normally requires greater than normal concentrations of antibiotics. Sometimes amputations are necessary to avoid blood poisoning when biofilms form.
- In addition to MRSA, the salve works against wound-infecting Acinetobacter baumanii, Stenotrophomonas maltophilia, S. epidermidis and S. pyogenes that are typical of diabetic foot ulcers that may develop sepsis and result in amputation of the foot.
- The most recent studies show that none of the individual ingredients alone have an effect on MRSA and that if you leave out any of the ingredients the salve is less successful at killing the superbugs.
- Natural medicines have always required mixing ingredients to get symbiotic reactions that improve the efficacy of the final product, while modern studies tend to try to isolate components and may miss important combinations.
- The researchers don’t know how the individual ingredients interact, but without all the ingredients in the prescribed quantities, the salve kills fewer bacteria.
- It is amazing that a millennium ago doctors had this remedy figured out and optimized.
- The bottom line is follow the recipe exactly to get the most impactful salve!

Old cauldrons. Credit: Caio Viana, CC BY-SA 4.0 <https://creativecommons.org/licenses/by-sa/4.0>, via Wikimedia Commons